FreesLab - Bacterial Pathogenesis and Antibiotic Resistance
The world-wide spread of antibiotic resistant bacteria represents one of the greatest threats to human and animal health. In the FreesLab we aim to identify novel targets that can be used to dis-arm bacteria by either restoring antibiotic sensitivity, or by preventing production of central virulence factors.
|
Our research is dedicated to unravel the molecular mechanisms underlying the ability of Staphylococcus aureus and other Gram-positive bacterial pathogens to cause disease and to develop antibiotic resistance. Focus has been on the highly conserved ClpP proteases and Clp chaperones that by controlling toxin production, stress responses, cell division and antiobiotic resistance are essential for the virulence of Staphylococcus aureus. |
Current work in the FreesLab focuses on elucidating the killing mechanism of penicillin and other antibiotics targeting the bacterial cell wall.
“Despite that these antibiotics are among the most prescribed antibiotics worldwide, the exact mechanisms leading to cell death are poorly understood. Delineating the killing mechanisms of these important antibiotics could yield new treatments options for multi-resistant pathogens”, says group leader Dorte Frees.
|
Research projects within FreesLab
Virulence gene regulation
Staphylococcus aureus produces a wide range of toxins that is uses to cause disease. Examples are the enterotoxins that cause food-poisoning, and TST-1 that causes the fatal disease toxic shock syndrome. Inactivation of the ClpXP protease abolished expression of most toxin genes and rendered S. aureus avirulent. ClpXP thus represents a promising target of antimicrobials, and a major aim of our research is to gain insight into the molecular mechanisms that link the ClpP protease to virulence gene regulation.
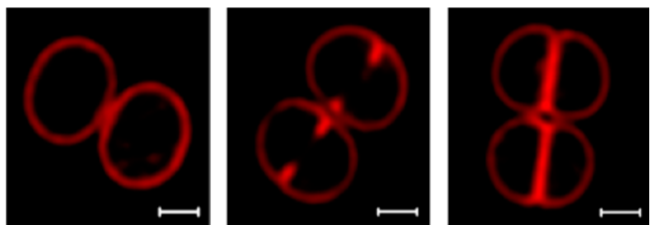
Coordination of cell wall synthesis and cell division
Cell division is required for growth of all bacterial populations and bacterial cell division proteins have attracted increasing interest as targets for antibiotics. The processes of cell division and septum formation need to be tightly co-ordinated in order to avoid cell lysis and we are currently investigating how the ClpX chaperone and the ClpXP protease contribute to these processes.
Last line defences against antibiotic resistant Staphylococcus aureus
The aim of the project is to elucidate how the chaperone ClpX contributes to development of resistance to the last line anti-staphylococcal agent daptomycin. Specifically, we will address if daptomycin resistance and immune escape mechanisms coevolve, thus increasing the likelihood of treatment failure.
Factors contributing to high level resistance towards cell-wall targeting antibiotics
Clinical MRSA isolates exhibit very different resistance levels and, interestingly, the variation in resistance levels does not correlate with expression of the resistance gene, mecA (encoding PBP2a), clearly demonstrating that intrinsic factors contribute to the resistance levels, and we are currently investigating some of these factors.
Extracellular vesicles as vehicles for toxins
The aim of this project is to use genetic approaches to investigate the molecular principles that govern membrane vesicle formation in S. aureus, and state-of-the-art quantitative proteomics to investigate the protein content of vesicles.
FTP

Group/project members
Internal researchers
| Name | Title | Phone | |
|---|---|---|---|
| Dorte Frees | Associate Professor | +4535332719 | |
| Gitte Petersen | Laboratory Technician | +4535336441 | |
| Vi Phuong Thi Nguyen | Laboratory Technician | +4535336426 |
Students
| Navn | Titel |
|---|---|
|
Julie Emdrup |
Master student |
|
Nidda Ilahi Piracha |
Master student |
|
Jakob Hjort West |
Master student |
|
Annie Justh |
Master student |

